|
Research Article
Primary transport on extracorporeal membrane oxygenation: Two Indian center experience
1 Department of Cardiac Anesthesiology & Critical Care and ECMO Services, Medica Superspecialty Hospital, Kolkata, India
2 Department of Cardiac Anesthesiology & Critical Care and ECMO Services, Medica Superspecialty Hospital, Kolkata, India
3 Department of Cardiac Anesthesiology & Critical Care and ECMO Services, Medica Superspecialty Hospital, Kolkata, India
4 Department of Cardiac Anesthesiology & Critical Care and ECMO Services, Medica Superspecialty Hospital, Kolkata, India
5 Department of Cardiac Anesthesiology & Critical Care and ECMO Services, Ridhivinayak Critical Care & Cardiac Center (RVCC), Mumbai, India
Address correspondence to:
Sandip Gupta
(ECMO Fellow, ESOI), MD (PEDIATRICS), Department of Cardiac Anesthesiology & Critical Care and ECMO Services, Medica Superspecialty Hospital, Kolkata,
India
Message to Corresponding Author
Article ID: 100021A05SG2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Gupta S, Chakraborty A, Sarkar K, Chatterjee D, Oza P. Primary transport on extracorporeal membrane oxygenation: Two Indian center experience. Edorium J Anesth 2021;7:100021A05SG2021.ABSTRACT
Aims: Extracorporeal membrane oxygenation (ECMO) can be a lifesaving modality for patients with severe reversible pulmonary and/or cardiac failure, but its use remains restricted to a few highly equipped referral centers. Conventional transports to an ECMO center can be hazardous. Transport teams are usually trained to transfer stable patients across hospitals. As ECMO patients are extremely sick, specially trained critical care teams to deal with all possible complications in these critically ill patients will be required. Therefore, many ECMO centers have developed transport programs with the mobile ECMO team. In this study, we aim to present a brief account of the two-center experience of ECMO transport from India.
Methods: Retrospective observational study is depicting the data of two mobile ECMO teams over 4 years, where 21 patients (16–74 years) were evaluated. Analysis was done for the transport arrangements, different characteristics of ECMO retrieval patients, their outcomes, and predictors of mortality of a total of 21 patients from two different referral centers of India. As it is a retrospective observational study, hence institutional ethical committee approval was waived off.
Results: The mean distance of travel was 87.24±104.5 km (range 2–250 km) and transportation was by road in all cases. About 38% (n=8/21), patients had suffered from complications during transport like hypotension, cardiac arrest. There were no deaths in connection with transportation. The overall mortality rate was 33.3% with no difference over gender, age, duration of pre-ECMO ventilation, or duration of transport. The most common indication associated with ECMO transport was H1N1 infection.
Conclusion: We found that patient transfer if done with proper protocols by a prepared team with full knowledge of problem areas to a referral institution while on ECMO support seems to be safe and adds no significant risk of mortality to ECMO patients.
Keywords: Acute respiratory failure, Extracorporeal membrane oxygenation, Mobile ECMO team, Retrieval, Transport
INTRODUCTION
Extracorporeal membrane oxygenation (ECMO) has become more and more recognized as a treatment modality for the treatment of refractory respiratory and/or cardiac failure [1],[2]. As only a few designated centers with expertise can provide ECMO support, hence the patients who require ECMO therapy need to be transported to these hospitals. Moreover, the critical nature of the illness makes conventional transport risky and susceptible to adverse events so often there is a need for cannulation at referring hospitals and then transporting patients on ECMO [3],[4],[5]. In the developed world, most specialized centers have a dedicated transport team for ECMO retrieval, thus ensuring the safety of the patients [6],[7]. In developing nations, like India, there has been a rapid rise in the use of ECMO in recent years, but data regarding ECMO transport is scarce. This study aims at describing a brief account of different characteristics of ECMO retrieval patients, their outcomes, and predictor of mortality of a total of 21 patients from two different centers in India, Medica Hospital, Kolkata, and Ridhivinayak Critical Care & Cardiac Center (RVCC), Mumbai.
MATERIALS AND METHODS
Data from both the hospitals were retrospectively collected from patient’s hospital charts, which are biometrically protected and stored in hospital servers. The additional data were obtained from the patient’s ambulance charts. We collected the following data: age group, gender, diagnosis, type of ECMO, time taken to transport, and distance traveled. As it is a retrospective observational study, hence institutional ethical committee approval was waived off.
Logistics
All 21 patients with pulmonary (n=18) or cardiac failure (n=3) were transported by ambulance by road from the local center to referral hospitals. All the transports from 2015 to September 2019 were included in this study.
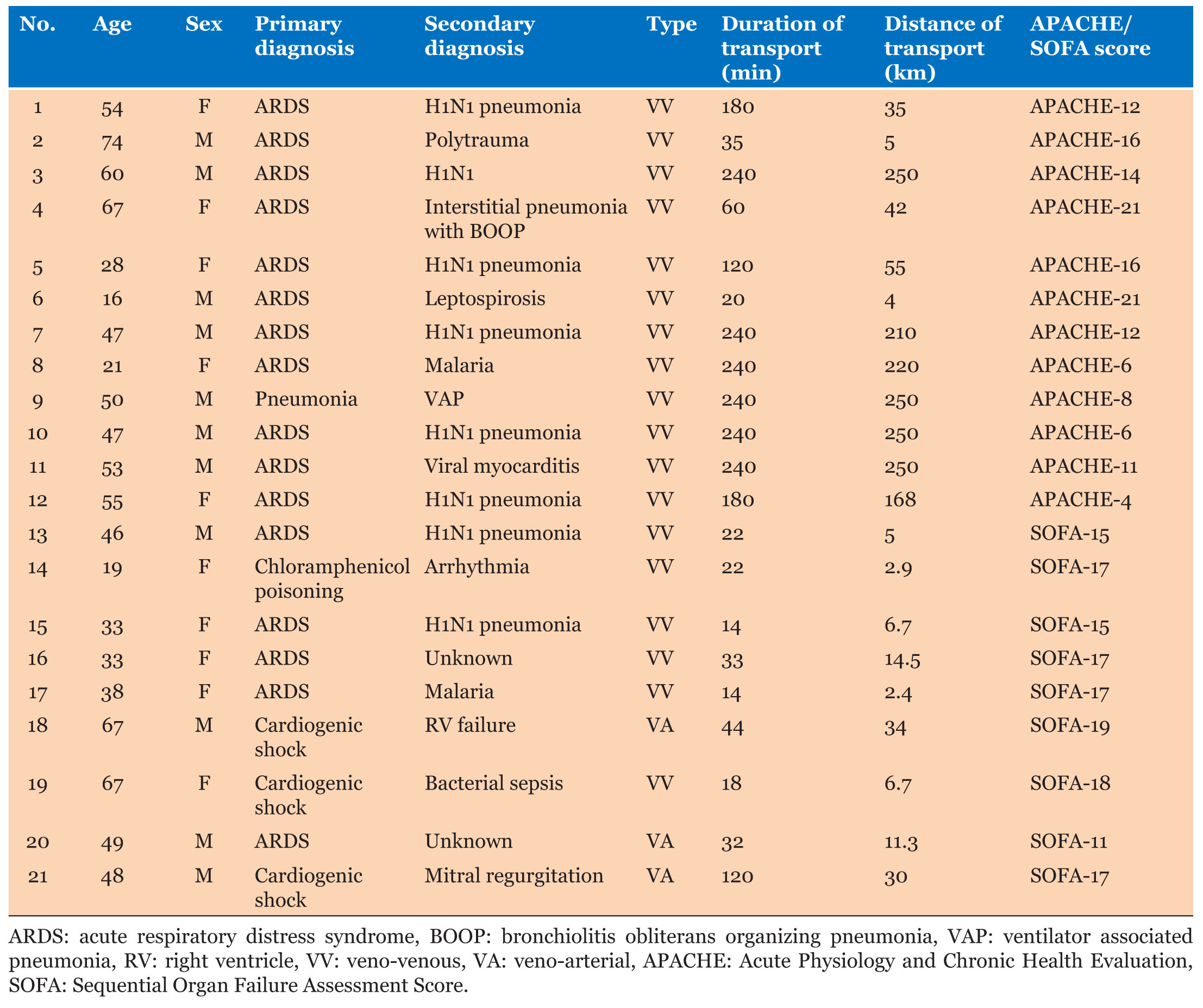
The study population consisted of patients from the age range of 16–74 years, with a mean age of 46.29±16.6. There were 10 females and 11 males. Diagnoses leading to initiation of ECMO were acute respiratory distress syndrome (ARDS) post-infectious/sepsis (n=15, 71.4%) ARDS post-trauma (n=1), cardiac failure (n=3, 14.3%) chloramphenicol poisoning (n=1), ventilator-associated pneumonia (n=1) as shown in Table 1.
The severity of illness of the patients was estimated using the SOFA scoring system at Medica Hospital, Kolkata, and APACHE II score at RVCC, Mumbai.
All the transport was done by ground ambulance. Upon receiving a retrieval request, the lead anesthetist/intensivist in the unit decided to accept or not, after collecting details candidacy for transport based on primary diagnosis, ventilator parameters, hemodynamic support of primary disease process, and neurological state and ruling out the exclusion criteria. If the patient was eligible, then the referring hospital was asked to do the counseling about the potential risk associated with both transport and ECMO support.
Percutaneous cannulation with the Seldinger technique was used by the intensivist to insert the catheter by both teams. Ultrasonography was routinely used to verify the patency of the blood vessels and the insertion of the cannula.
ECMO team
We did have a special transport team dedicated to ECMO retrievals at both centers. At Medica, two senior intensivists, a perfusionist, and an ECMO nurse specialist were part of the team. At RVCC, the transport team included a single senior intensivist, two nursing staff, and a perfusionist. Upon reaching the ECMO center, on-site re-evaluation of the patient was done and, the need for ECMO, mode of ECMO, and cannulation approach was decided. Then after brief reinforced counseling, the retrieval team had performed the cannulation, started on ECMO support, and transported back to the referral center.
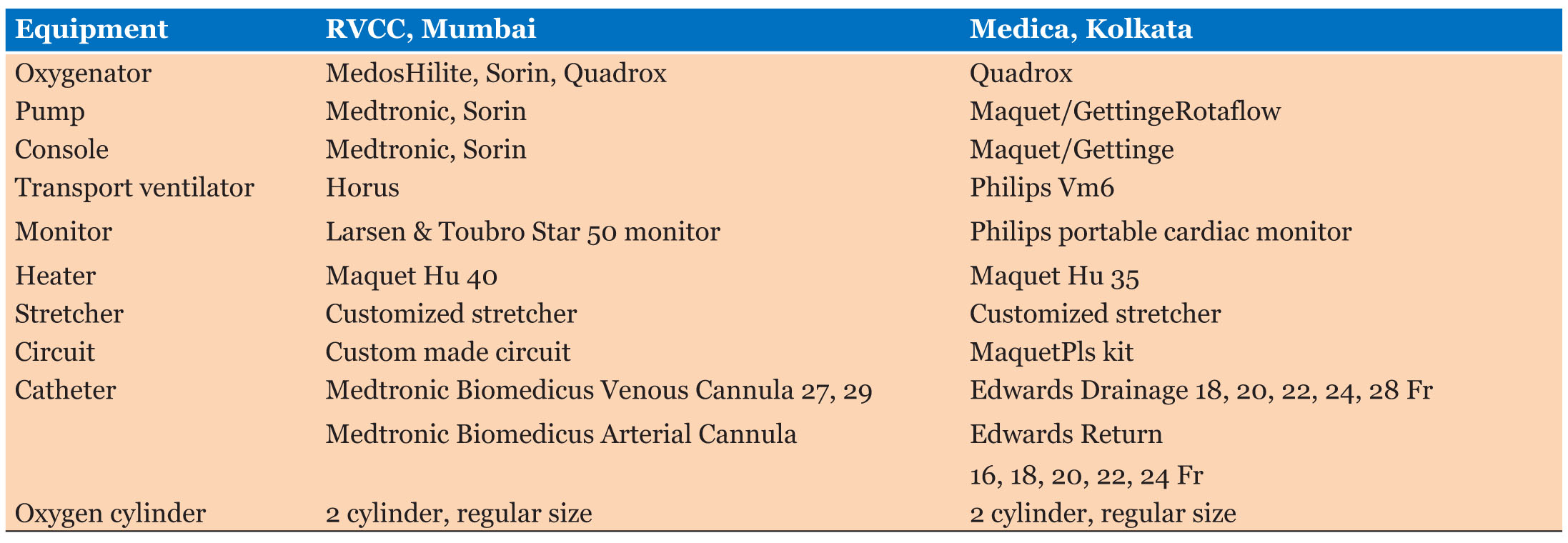
Transport equipment
ECMO transport is an emergency, hence all the required equipment was packed and kept ready in a storage section of ICU, with additional backup equipment such as circuits and cannula for safety in case of any adverse events. Table 2 summarizes the transport types of equipment used in the ambulances of both centers.
Data collection and analysis
Transport services were started in Medica, Kolkata on 03/02/2015 and in RVCC, Mumbai on 02/05/2012. Data collected here summarizes the transports done in both centers till August 2019. Data were obtained from our database and patients’ records and ambulance charts. We collected the following data: age, group, gender, diagnosis, types of ECMO.
Statistical methods
SPSS 16 software (copyright 2007, SPSS Inc., Chicago, IL, USA) was used for data analysis. For frequency percentages, an independent t-test for continuous variables and the chi-square test/Fisher’s exact test for categorical variables were applied. A p-value < 0.05 was considered significant.
RESULTS
The characteristics of the study population have been depicted in Table 1. The average distance of travel was 87.24 km (median: 30 km; range 2–250 km) and transportation was by road in all cases. There were no deaths in connection with transportation. Veno-venous (VV) ECMO was used in 17/21 (80.95%) patients whereas veno-arteria (VA) ECMO was required in 4/21 (19.05%).
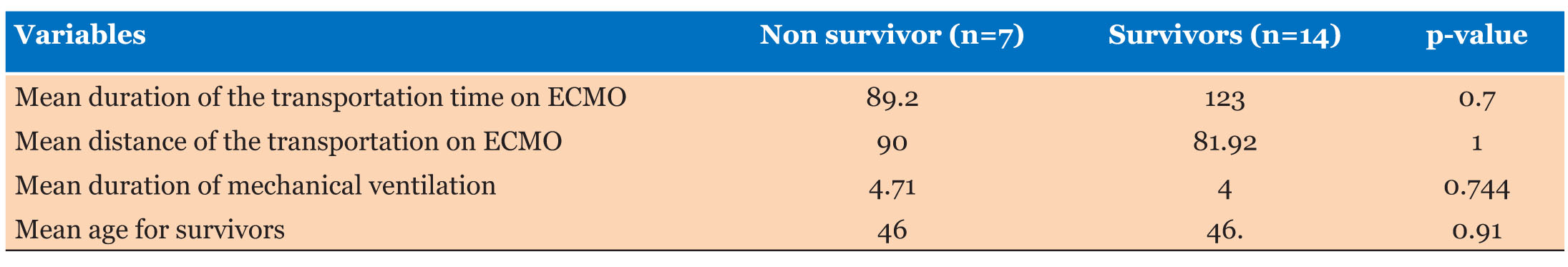
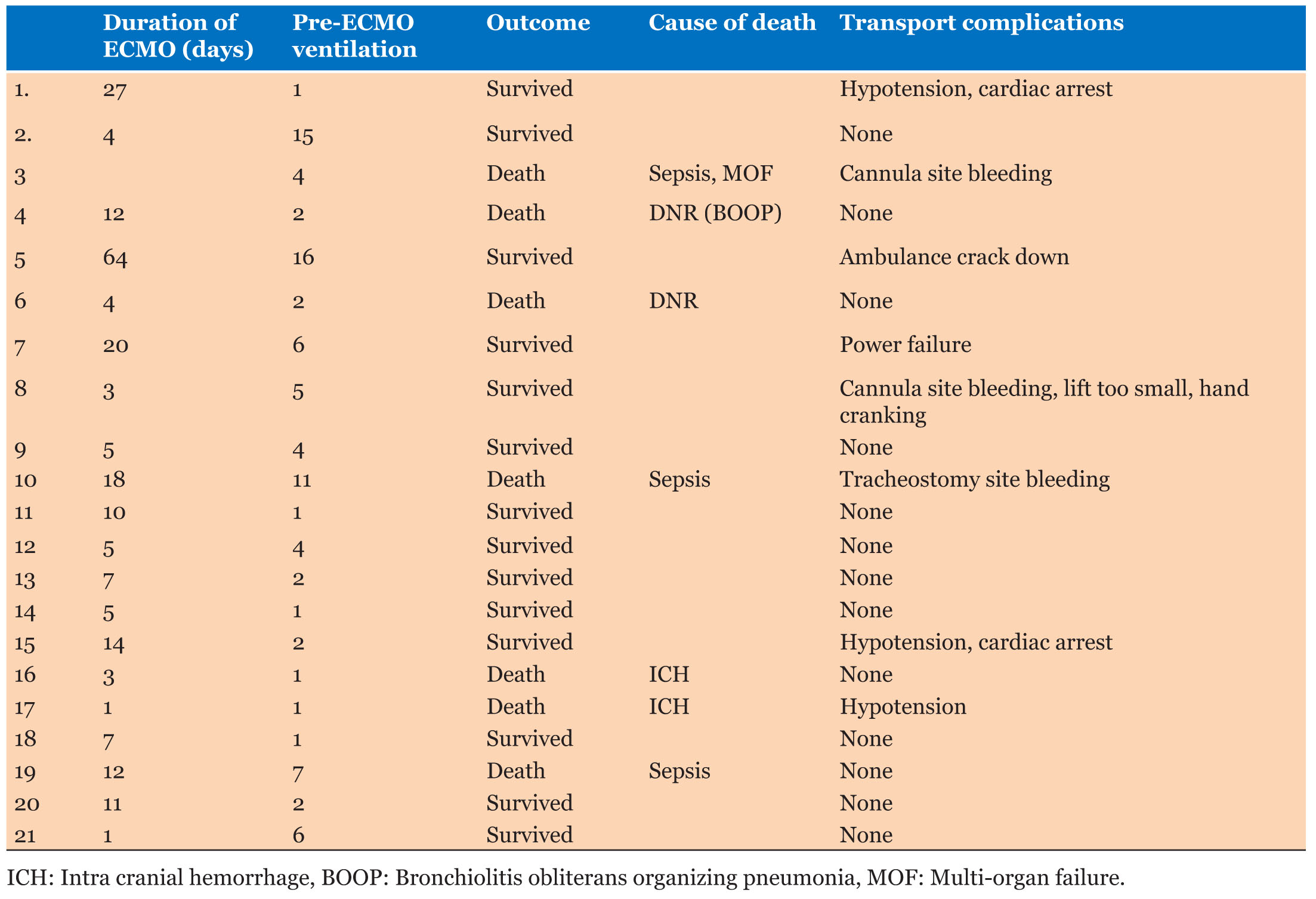
As shown in Table 3, after an average of 11.9 days (median: 7 days; range 1–64 days), 14 patients (67%) could be weaned from ECMO, while 7 patients (33%) died on ECMO. Mean ECMO time for those who died was 10.7 (median: 7) versus 12.5 days (median: 7) for survivors, p=0.78. There were no differences in early mortality related to gender. In the male 8 out of 11 survived, whereas in females 6 out of 10 had survived, p=0.87.
The mean age for survivors was 46 (median: 48.5; range: 19–74) versus 46.8 (median: 47; range: 16–67) years in fatal cases, p=0.91. The average duration of the transportation time on ECMO back to the hospital was 123 minutes (median: 120 min; range: 14–240 minutes) in survivors and 89.2 minutes (median: 33; range: 14–240 minutes) in non-survivors, p=0.70. The average distance of the transportation on ECMO by ambulance was 91.63 kilometers (km) (median: 34.5; range: 2.9–250 km) in survivors and 81.37 km (median: 14.5 and range: 2.4–250 km) in non-survivors, p=1.0 with no statistical significance of the difference between the two groups.
Duration of mechanical ventilation before ECMO was 4.71 days (median: 3 days; range: 1–16 days) hours in survivors and 4 days (median: 2 days and range: 1–13 days) in the non-survivors p=0.744. Among the etiologies, the most common cause was H1N1 infection which was present in 8/21 (38%), sepsis in 3/21, and malaria in 2/21 patients.
As shown in Table 4, out of a total of 20 patients, 8 (38%) patients had suffered from complications during transport like hypotension (n=3/21), cardiac arrest (n=2/21), cannulation site bleeding (n=2/21), tracheostomy bleeding (n=1/21), ambulance breakdown (n=1/21), power failure (n=1/21), hand cranking (n=1/21), lack of space in the lift (n=1/21). Complications during transport were not associated with ICU mortality.
DISCUSSION
ECMO is a lifesaving procedure for patients with refractory respiratory and/or cardiac failure, with only specialized centers providing ECMO, hence patients need to be shifted to these designated ECMO centers. Patients needing ECMO, in general, are too critical to be transported even on maximum ventilator settings and other intensive care support. Hence, there has been an increasing trend of cannulating the patient in the referring center and then transporting them on ECMO with the help of a mobile ECMO team [2],[3],[4].
Moreover, data from extracorporeal life support organization (ELSO) registry suggests that centers doing high volume ECMO experience have significantly lower mortality than units with lesser experience [8],[9]. This volume-mortality association has favored the development of the policy of developing centralize ECMO treatment rather than starting the ECMO program in multiple centers, the classical example being the current National ECMO service provision in England, where each of the five specialist ECMO centers supports a large number of regional hospitals, 24×7 with help of a well-equipped mobile ECMO team [10],[11].
The development of specialized ECMO teams and retrieval in developing countries like ours is in the nascent stage. In this study, we described the recent experience of ECMO transport from two high-volume ECMO centers in India. Patients were referred to both hospitals due to serious lung or heart failure. So far, in India, the majority of transportations on ECMO support are by road in the ambulance. All transports were performed without any deaths reported during transportation. This is in agreement with other reports [12],[13] [14],[15]. None of the later deaths were related to transportation.
Overall survival till discharge in patients transported on ECMO was 66.7% and is comparable to the overall ECMO survival rate of 55% in ELSO data [16]. It is also comparable to the Swedish study by Lindén et al. [17], and Norway study by Wagner et al. [18], showing a survival rate of 72% and 66.7% respectively in patients needing transportation on ECMO. There was no difference in mean age, distance traveled and time of transport, pre-ECMO ventilation, and the total duration of ECMO support among the survivors and non-survivors (Table 3). In our study, 38% (8/21) of the patients had developed complications during transport which was similar to 28% as observed in a Swedish study by Fletcher-Sandersjöö et al. [12].
Limitations of our study include the retrospective nature of data and small sample size for statistical analysis, as well as the use of different scoring systems in the studies, which makes it difficult to compare expected mortality with final results. However, as previously described, the overall mortality rate was compatible with the expected mortality previously published in the ELSO registry.
CONCLUSION
Our limited data tends to support the growing evidence, in favor of transportation of patients with refractory respiratory and/or cardiac failure on ECMO by cannulating them at the referring center. Life-threatening situations can occur during mobile ECMO transport, needing immediate intervention by highly skilled and experienced personnel and transport needs to be organized accordingly. Overall, the availability of a mobile ECMO team makes transport to a referral institution while on ECMO support safe and adds no significant risk of mortality to ECMO patients.
REFERENCES
1.
Gerke AK, Tang F, Cavanaugh JE, Doerschug KC, Polgreen PM. Increased trend in extracorporeal membrane oxygenation use by adults in the United States since 2007. BMC Res Notes 2015;8:686. [CrossRef]
[Pubmed]

2.
McCarthy FH, McDermott KM, Kini V, et al. Trends in U.S. extracorporeal membrane oxygenation use and outcomes: 2002–2012. Semin Thorac Cardiovasc Surg 2015;27(2):81–8. [CrossRef]
[Pubmed]

3.
Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicentre randomised controlled trial. Lancet 2009;374(9698):1351–63. [CrossRef]
[Pubmed]

4.
Boedy RF, Howell CG, Kanto WP Jr. Hidden mortality rate associated with extracorporeal membrane oxygenation. J Pediatr 1990;117(3):462–4. [CrossRef]
[Pubmed]

5.
Noah MA, Peek GJ, Finney SJ, et al. Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A (H1N1). JAMA 2011;306(15):1659–68. [CrossRef]
[Pubmed]

6.
Forrest P, Cheong JY, Vallely MP, et al. International retrieval of adults on extracorporeal membrane oxygenation support. Anaesth Intensive Care 2011;39(6):1082–5. [CrossRef]
[Pubmed]

7.
Forrest P, Ratchford J, Burns B, et al. Retrieval of critically ill adults using extracorporeal membrane oxygenation: An Australian experience. Intensive Care Med 2011;37(5):824–30. [CrossRef]
[Pubmed]

8.
Coppola CP, Tyree M, Larry K, DiGeronimo R. A 22-year experience in global transport extracorporeal membrane oxygenation. J Pediatr Surg 2008;43(1):46–52. [CrossRef]
[Pubmed]

9.
Barbaro RP, Odetola FO, Kidwell KM, et al. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med 2015;191(8):894–901. [CrossRef]
[Pubmed]

10.
Critical care services. [Available at: https://www.england.nhs.uk/commissioning/ccs/]

11.
Extracorporeal membrane oxygenation for severe acute respiratory failure in adults. 2011. [Available at: https://www.nice.org.uk/guidance/ipg391]

12.
Fletcher-Sandersjöö A, Frenckner B, Broman M. A single-center experience of 900 interhospital transports on extracorporeal membrane oxygenation. Ann Thorac Surg 2019;107(1):119–27. [CrossRef]
[Pubmed]

13.
Cianchi G, Lazzeri C, Bonizzoli M, et al. The 8-year experience of the Florence referral ECMO center and retrieval team for acute respiratory failure. J Cardiothorac Vasc Anesth 2018;32(3):1142–50. [CrossRef]
[Pubmed]

14.
Mendes PV, de Albuquerque Gallo C, Besen BAPM, et al. Transportation of patients on extracorporeal membrane oxygenation: A tertiary medical center experience and systematic review of the literature. Ann Intensive Care 2017;7(1):14. [CrossRef]
[Pubmed]

15.
Droogh JM, Smit M, Absalom AR, Ligtenberg JJM, Zijlstra JG. Transferring the critically ill patient: Are we there yet? Crit Care 2015;19(1):62. [CrossRef]
[Pubmed]

16.
Extracorporeal Life Support Organization—ECLS Registry Report. 2020. [Available at: http://www.elso.org/Registry/Statistics/InternationalSummary.aspx]

17.
Lindén V, Palmér K, Reinhard J, et al. Inter-hospital transportation of patients with severe acute respiratory failure on extracorporeal membrane oxygenation – national and international experience. Intensive Care Med 2001;27(10):1643–8. [CrossRef]
[Pubmed]

18.
Wagner K, Sangolt GK, Risnes I, et al. Transportation of critically ill patients on extracorporeal membrane oxygenation. Perfusion 2008;23(2):101–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Sandip Gupta - Substantial contributions to conception and design, Analysis of data, Interpretation of data, Drafting the article, Final approval of the version to be published
Arpan Chakraborty - Acquisition of data, Analysis of data, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Kunal Sarkar - Acquisition of data, Analysis of data, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Dipanjan Chatterjee - Acquisition of data, Analysis of data, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Pranay Oza - Substantial contributions to conception and design, Acquisition of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Sandip Gupta et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.